Pneumothorax
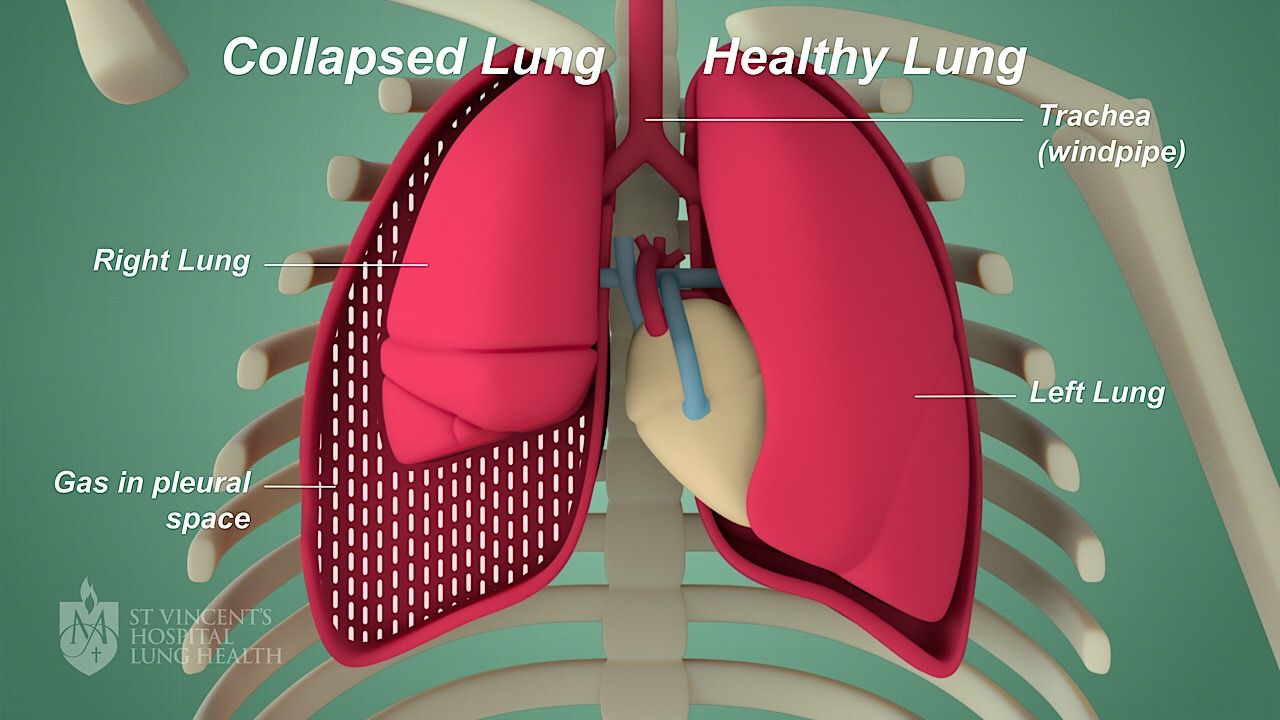
A pneumothorax is when the lung has collapsed due to air entering the space around your lungs (known as the pleural space).
What is a pneumothorax?
What causes a pneumothorax?
What are the signs and symptoms of a pneumothorax?
What are the possible tests to diagnose a pneumothorax?
What are the possible treatments for a pneumothorax?
What is the future plan if I’ve had a pneumothorax?
What is a pneumothorax?
A pneumothorax is when the lung has collapsed due to air entering the space around your lungs (known as the pleural space). Air can enter the pleural space through an opening in your chest wall or in the lung. Air in the pleural space creates an increase in pressure around the lung and causes it to collapse.
A pneumothorax can be severe, depending on how much air is trapped in the pleural space. A small amount of trapped air can usually resolve by itself, provided there are no other complications. Larger amounts of trapped air can be serious and lead to death if medical treatment is not obtained.
The image below shows a pneumothorax. (Click image to enlarge)
What causes a pneumothorax?
There are four types of pneumothorax.
Primary spontaneous pneumothorax
Primary spontaneous pneumothorax occurs in young people (aged 15-34) without any history of lung disease. Whilst the cause is not well understood, people at risk include smokers, tall men and those who have had a family member with a pneumothorax.
Secondary spontaneous pneumothorax
Secondary spontaneous pneumothorax typically occurs in people who have pre-existing connective tissue disorders (such as Marfan’s Syndrome) or lung diseases such as COPD (chronic obstructive pulmonary disease), cystic fibrosis, tuberculosis, pneumonia, lung cancer, sarcoidosis, pulmonary fibrosis or cystic lung diseases (such as lymphangioleiomyomatosis - LAM).
Traumatic pneumothorax
Traumatic pneumothorax occurs from a traumatic injury to the chest or wall of the lung, usually from an accident or through a contact sport. Traumatic injuries can include:
- Changes in air pressure (ie scuba diving or climbing at altitude)
- Fractured ribs
- Injury to the chest as a result of contact sport (ie tackle in rugby)
- Medical procedures that damage the lung (such as a lung biopsy or use of a ventilator)
- Stab or bullet wounds.
Tension pneumothorax
Tension pneumothorax is a life-threatening condition that requires immediate treatment. Air cannot escape the pleural space, so every time the person breathes in, more air enters the space, increasing the pressure on the lung and heart. A tension pneumothorax is more likely to occur with trauma, such as a knife wound to the chest.
What are the signs and symptoms of a pneumothorax?
Symptoms of a traumatic pneumothorax typically occur during the period of trauma or just after. In contrast, symptoms of a spontaneous non-traumatic pneumothorax usually occur when the person is at rest. Sudden, severe chest pain is often the first symptom of a pneumothorax. Other symptoms include:
- Abnormally fast heart rate (known as tachycardia)
- Blue-tinged lips and skin
- Breathlessness on exertion
- Cold sweats
- Constant ache and tightness in the chest
- Difficulty catching your breath
- Sharp pain when breathing in, with fast and shallow breathing.
What are the possible tests to diagnose a pneumothorax?
Diagnosis of a pneumothorax is typically done via a chest X-ray, which takes images to detect the presence of air in the pleural space (area round the lungs). A CT scan and thoracic ultrasound can also be used to help diagnose a pneumothorax.
What are the possible treatments for a pneumothorax?
Treatment for a pneumothorax will depend on your symptoms, medical history and the severity of the pneumothorax. Treatment options can be both surgical and non-surgical and can include:
- Chest drain insertion – can be used to help remove excess air in the pleural space, enabling your lungs to expand fully again
- Observation – is usually appropriate for people who have a primary spontaneous pneumothorax and who don’t have difficulty breathing; ongoing chest X-rays may be recommended to monitor lung function and to ensure all air from the pleural space has disappeared and the lungs can fully expand again, and it is recommended to avoid all contact sport and any activity, like air travel, that could impact on healing the pneumothorax
- Pleurodesis – is a procedure which sticks the lung to the chest cavity; it is often recommended for people who have had previous pneumothorax to help prevent further collections of air in the pleural space, or in people with a chest drain and an ongoing leak of air that has not settled after a few days
- Surgery – there are several types of surgery for pneumothorax:
- Thoracoscopy (also known as video-assisted thoracoscopic surgery or VATS) – is where a small camera is placed in the wall of your chest to help determine the best treatment; possibilities post-surgery include closing up blisters and air leaks, or removing a portion of the lung that has collapsed (called a lobectomy)
- Thoracotomy – where an incision is made in the pleural space to help determine a suitable treatment option.
What is the future plan if I’ve had a pneumothorax?
Generally, you can see improvements from a pneumothorax as early as a few days after treatment. There is a risk of having another pneumothorax (because you have already had one), so if symptoms occur again it is important to seek medical attention straight away.
Depending on the type and severity of your pneumothorax, you may require follow-up monitoring with chest X-rays. You may also need to avoid air travel as instructed by your medical team. If you smoke, talk to your doctor about ways to quit, as smoking increases your risk for subsequent pneumothoraces.